Fitness
Test-treat-track-test-treat (5T) approach for Schistosoma haematobium elimination on Pemba Island, Tanzania – BMC Infectious Diseases

Participation in school-based and household-based surveys 2021 and 2022
The number of children and household members enrolled and the overall results of the baseline school-based and household-based survey, respectively, in all 20 IUs carried out from November 2020 to February 2021 are presented elsewhere [18]. This baseline survey revealed a total of five hotspot IUs according to the pre-set prevalence threshold criteria. Additional 15 IUs were identified as low-prevalence, including 11 low-prevalence primary schools (no primary school was located in four IUs) and 15 low-prevalence communities. Subsequent results focus on these 11 low-prevalence primary schools and 15 low-prevalence communities, since the 5T interventions that are the primary focus of this publication were only implemented in the low-prevalence IUs.
In the school-based survey conducted in 2021, a total of 1924 children were registered across the 11 low-prevalence schools. Of these 1924 children, 332 (17.3%) were absent on the day of urine collection, and 32 (1.7%) refused to participate or did not provide a signed consent form, resulting in 1560 (81.1%) children providing a fresh urine sample for examination (Supplementary File 1: Fig. 1A).
In the household-based survey in 2021, 3539 household members were registered across the 15 low-prevalence communities. Of these 3539 household members, 564 (15.9%) were absent on the day of urine collection, refused to participate, or did not provide a signed consent form. Hence, a total of 2975 (84.1%) household members provided a fresh urine sample for examination (Supplementary File 1: Fig. 1A).
In the school-based survey in 2022, a total of 1898 children were registered across the 11 low-prevalence schools. Of these 1898 children, 238 (12.5%) were absent on the day of urine collection, and 15 (0.8%) refused to participate or did not provide a signed consent form. Hence, 1645 (86.7%) children provided a fresh urine sample for examination (Supplementary File 1: Fig. 1B).
In the household-based survey in 2022, 3683 household members were registered across the 15 low-prevalence communities. Of these 3683 household members, one (0.03%) person was excluded due to ineligibility (age 1B).
Demographic information from participants of all surveys and interventions is shown in Table 1.
Participation in the 5T intervention period in 2021
Between May and October 2021, a total of 4283 and 777 children were registered in 11 schools and 15 madrassas, respectively, across the 15 low-prevalence IUs (Fig. 1). Of the 4283 children registered in the primary schools, 540 (12.6%) were absent on the day of urine collection and 39 (0.9%) refused to participate or did not provide a signed consent form. Hence, 3704 (86.5%) children were tested for microhematuria and included in the analysis. Of the 777 children registered in the madrassas, 164 (21.1%) were absent on the day of urine collection, and 19 (2.4%) refused to participate or did not provide a signed consent form. Hence, a total of 594 (76.4%) children were tested for microhematuria and included in the analysis.
Of the 3704 children tested in primary schools and 594 children tested in madrassas, 190 (5.1%) and 47 (7.9%), respectively, were microhematuria-positive.
Of the 237 microhematuria-positive children, 215 (90.7%) were tracked to 200 households. In 89 (44.5%) of the 200 households, nobody was present at the time of visit or all present members refused to participate. In the remaining 111 households, of the 280 household members present at the time of the visit, 22 (7.9%) refused to participate or did not provide a signed consent form. A total of 258 (92.1%) household members provided a fresh urine sample and had demographic data recorded.
Of the 237 microhematuria-positive children, 189 (79.7%) were tracked to 61 water bodies. At 15 water bodies, a total of 61 individuals were present at the time of the visit. Of the 61 individuals, one (1.6%) person refused to participate or did not provide a signed consent form. A total of 60 (98.4%) individuals provided a fresh urine sample and had demographic data recorded.
Information about sex and median age of the study participants, stratified per survey and intervention period, is indicated in Table 1.
Microhematuria and Schistosoma haematobium prevalence in surveys, test-treat-track-test-treat intervention period, and health facilities
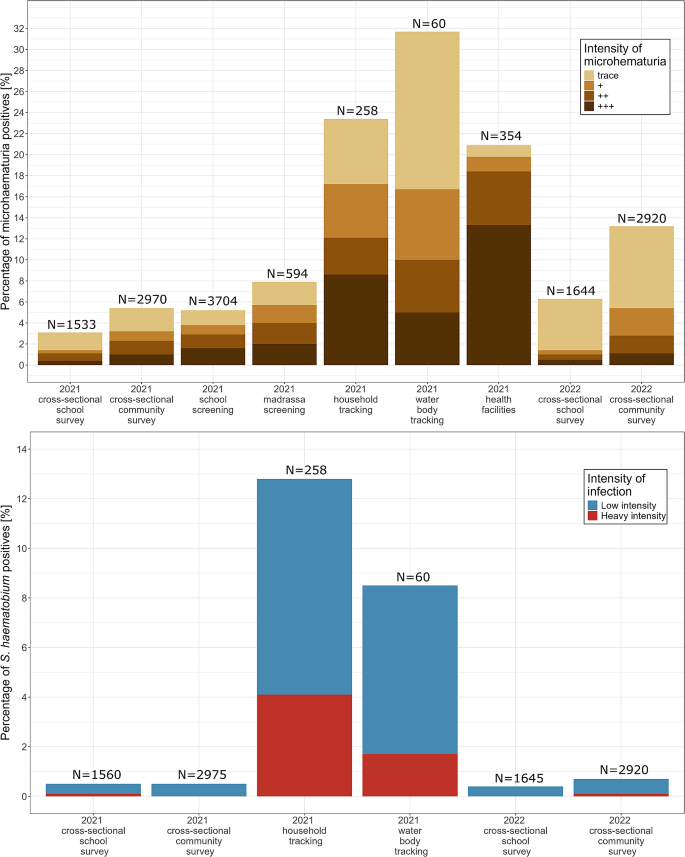
The overall prevalence of microhematuria among children who participated in the school-based surveys in the 15 low-prevalence IUs was 3.1% (47/1533; 95% CI: 2.3–4.1) in 2021 and 6.3% (104/1644; 95% CI: 5.2–7.6) in 2022 (Fig. 2A and Supplementary File 2: Table 1). The results of the two-sample proportion test showed that the prevalence between the two years was significantly different (p p
The prevalence of microhematuria excluding trace results among children who participated in the school-based surveys in the 15 low-prevalence IUs was 1.4% (21/1533; 95% CI: 0.9–2.1) in 2021 and 1.5% (24/1644; 95% CI: 1.0–2.2) in 2022. The results of the two-sample proportion test showed that the prevalence between the two years was not significantly different (p = 0.93). The prevalence of microhematuria among participants of the household-based survey was 3.3% (98/2975; 95% CI: 2.7–4.0) in 2021 and 5.4% (159/2920; 95% CI: 4.6–6.3) in 2022. The results of the two-sample proportion test showed that the prevalence between the two years was significantly different (p
Figure 2B shows that the overall S. haematobium prevalence, as assessed in the school-based surveys, was 0.5% (7/1560; 95% CI: 0.2–1.0) in 2021 and 0.4% (6/1645; 95% CI: 0.2–0.9) in 2022 in schoolchildren attending the 11 primary schools of the 15 low-prevalence IUs. The results of the two-sample proportion test showed that the prevalence between the two years was not significantly different (p = 0.87). The S. haematobium prevalence, assessed in the household-based survey in the communities of the 15 low-prevalence IUs, was 0.5% (14/2975; 95% CI: 0.3–0.8) in 2021 and 0.7% (19/2920; 95% CI: 0.4–1.1) in 2022. The results of the two-sample proportion test showed that the prevalence between the two years was not significantly different (p = 0.41).
During the 5T intervention period in 2021, 5.1% (190/3704) of the children tested in primary schools and 8.0% (47/594) of the children tested in madrassas were microhematuria-positive (Fig. 2A). Of the 190 and 47 children tested positive for microhematuria in schools and madrassas, 180 (95.0%) and 42 (89.4%), respectively, were treated with praziquantel after testing. In the households and at the water bodies identified by tracking these microhematuria-positive children, 23.3% (60/258) and 31.7% (19/60), respectively, of the tested individuals were microhematuria-positive. Of the 60 and 19 individuals who tested positive in households and at water bodies, 98.3% (59/60) and 94.7% (18/19), respectively, were treated at the point-of-care.
The risk-based tracking of microhematuria-positive children from primary schools or madrassas to their homes identified 12.8% (31/243) of household members present at home at the time of the visit as S. haematobium egg-positive (Fig. 2B). At the water bodies that were identified by tracking microhematuria-positive children, 8.5% (5/60) of individuals present at the water bodies at the time of the visit were tested S. haematobium egg-positive.
Between August and November 2021, 354 patients presented with symptoms aligning with urogenital schistosomiasis in 13 of the 22 health facilities in the study area. All 354 individuals were tested with Hemastix reagent strips at the point-of-care. Among them, 20.9% (74/354) were microhematuria-positive (Fig. 2A). Of these 74 individuals, 90.5% (67/74) were treated with praziquantel in the health facilities.
Information on microhematuria and S. haematobium prevalence for each of the surveyed, tested and tracked populations, stratified by sex, are presented in Supplementary File 2: Table 1.
Microhematuria (A) and Schistosoma haematobium (B) prevalence in 15 low-prevalence implementation units in Pemba, Tanzania, in 2021–2022. The y-axis represents the percentage of positive-tested individuals for microhematuria (A) or S. haematobium infection (B). Colors indicate the grading of microhematuria or intensity of S. haematobium infections. N indicates the overall number of tested individuals per bar
Heterogeneity of microhematuria and S. haematobium prevalence during the test-treat-track-test-treat intervention period
The testing during the 5T intervention period showed a varying microhematuria prevalence between 0.0% and 15.6% in schools and between 0.0% and 30.0% in madrassas (Fig. 3A). The school and madrassa with the highest microhematuria prevalence were located in the same IU. During the risk-based tracking of children who tested positive for microhematuria in schools and madrassas, the microhematuria prevalence per IU varied between 0.0% and 47.6% in households and between 0.0% and 56.2% at water bodies, respectively.
In the 5T intervention period, the S. haematobium prevalence per IU ranged from 0.0 to 40.0% in households and from 0.0 to 25.0% at the water bodies, respectively (Fig. 3B).
In the test-and-treat intervention in the health facilities, the microhematuria prevalence ranged from 0.0 to 100% in health facilities (Fig. 3A). However, it should be noted that all health facilities with a microhematuria prevalence of 100% had tested
Microhematuria (A) and Schistosoma haematobium (B) prevalence in 15 low-prevalence implementation units in Pemba, Tanzania, in 2021. The y-axis represents the prevalence of microhematuria (A) or S. haematobium infection (B); each point represents one school/community. Colors indicate the grading of microhematuria or S. haematobium intensity infections, respectively, per school/community. The asterisk (*) denotes points where the prevalence was calculated with
Children tested in madrassas during the test-treat-track-test-treat activities
Of the 594 madrassa students who were tested for microhematuria, 219 (36.9%) attended a primary school that was part of our 5T interventions, but were enrolled in grades where screening for microhematuria was not operated, i.e., in nursery school, grades 1, 2, or grade 6. Another 79 (31.3%) of the 594 tested madrassa students reported that they would not visit a school. For 132 (22.2%) children, no information was available on their primary/secondary school enrolment and attendance because the assessment of primary school enrolment was only started from the third madrassa onwards. Another 97 (16.3%) of the 594 madrassa students were enrolled in primary schools that were not part of the SchistoBreak study schools. A total of 51 (8.6%) children were enrolled in grades 3–5 in one of the SchistoBreak study schools but were not present on the testing days, and 16 (2.7%) children were enrolled in secondary schools, which were not part of our 5T interventions. Of the 79 non-school attendees, 5 (6.3%) children were tested microhaematuria-positive. The microhaematuria prevalence in school attendees tested in madrassas was 9.1% (35/383).
Households and water bodies identified during the test-treat-track-test-treat interventions
The households of microhematuria-positive children were located between 8 and 4794 m (mean: 958 m) from the school or madrassa where the children were tested. Of the 215 children who were tracked to their homes, 71 (32.0%) children lived in households not located in the same IU as the school the children were attending (Fig. 4).
The water bodies indicated by microhematuria-positive children were located between 62 m and 10.1 km (mean: 1210 m) away from the school or madrassa where the children were tested. For 27.2% (43/158) of the positive-tested children, the water bodies they frequented were not located in the same IU as the screened school. Moreover, several water bodies were located at borders between two IUs and borders to shehias outside of the study area.
In two schools and five madrassas, respectively, no child tested positive for microhematuria, and therefore, no child was tracked to household or water bodies.
Spatial distribution of tracked households and water bodies. Spatial distribution of households of microhematuria-positive children and water bodies used and indicated by microhematuria-positive children emanating from the school/madrassa where the children were tested in the 15 low Schistosoma haematobium prevalence implementation units in the North of Pemba, Tanzania, in 2021. The locations of households are geographically masked in order to preserve confidentiality
Individuals treated and praziquantel tablets used during the mass drugs administration in 2020 and the 5T interventions in 2021
During the MDA in August 2020, 39,312 individuals were treated with praziquantel in the communities and schools of the 15 IUs that were identified as low-prevalence IUs in 2021 (Table 2). To treat these individuals, 78,853 praziquantel tablets were used, with an average of 2 tablets per treated person. During the 5T interventions in 2021, 336 individuals were treated in primary schools, madrassas, at households and at water bodies in the 15 low-prevalence IUs. For the 336 individuals, 1123 praziquantel tablets were used, with an average of 3 tablets per treated person. Hence, during the MDA in August 2020 around 70 times as many praziquantel tablets were used as during the targeted 5T interventions in 2021 in the same IUs. An additional 85 praziquantel tablets were used to treat 31 hematuria-positive individuals in the health facilities across the study area.