Fitness
Bowel Prep Quality Affects Long-Term Colonoscopy Outcomes
TOPLINE:
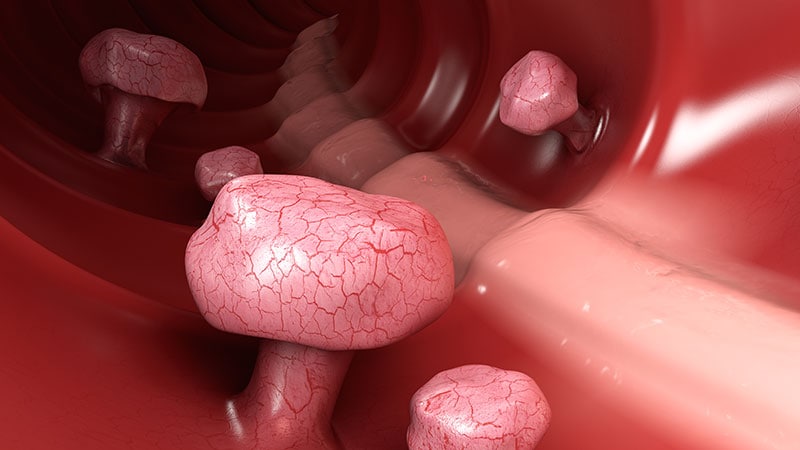
Individuals with fair or worse bowel preparation have lower adenoma detection rates and a higher risk for postcolonoscopy colorectal cancer (PCCRC) death, new data showed.
METHODOLOGY:
- Few large studies have investigated the degree of bowel preparation with long-term colorectal cancer (CRC) outcomes.
- Researchers analyzed data from 335,466 individuals aged 50 years and older who underwent screening colonoscopy in Austria over 10 years (2012-2022).
- Bowel preparation quality was assessed using the five-point Aronchick scale and categorized as excellent, good, fair, poor, or inadequate.
- Logistic regression and time-to-event analyses were used to assess the impact of bowel preparation quality on adenoma detection and PCCRC mortality.
TAKEAWAY:
- Bowel prep was excellent in 37% of procedures, good in 48%, fair in 11%, poor in 3%, and inadequate in 1%.
- With worsening degrees of bowel prep, the odds of detecting an adenoma, high-risk polyp, sessile serrated lesion (SSL), or traditional serrated adenoma (TSA) decreased significantly.
- For patients with inadequate bowel preparation, the odds ratio for detection was 0.44 for adenomas and 0.53 for SSL or TSA.
- The risk of dying from PCCRC was more than twofold higher with fair or poor bowel prep and more than fourfold higher with inadequate prep.
- Cumulative 10-year CRC mortality was 0.14% for excellent/good bowel preparation vs 0.41% for fair or worse preparation.
IN PRACTICE:
“Our findings further support the evidence that bowel preparation is a crucial element of high-quality colonoscopy that affects CRC outcomes in screening participants. Efforts should be made to increase bowel cleansing above fair scores,” the authors concluded.
SOURCE:
The study, led by Jasmin Zessner-Spitzenberg, MD, from the Division of Gastroenterology and Hepatology at the Medical University of Vienna, Vienna, was published online in the American Journal of Gastroenterology.
LIMITATIONS:
The researchers lacked data on CRC risk factors and information on surveillance colonoscopies, which could bias the results. Bowel preparation solutions and preferences of endoscopists, or whether split dosing was applied, were unknown, which limits insights into variations in preparation effectiveness.
DISCLOSURES:
The study was supported by the Main Association of Statutory Insurance Institutions, The Austrian Society for Gastroenterology and Hepatology, and the Austrian Cancer Aid. Zessner-Spitzenberg had no relevant disclosures. Other participating authors disclosed competing interests in the form of advisory roles, grant/research support, and speaker fees received from industry and academic institutions.










