Fitness
Anticipating Tricuspid Valve Regurgitation
PARIS — By assessing residual regurgitation after a transcatheter tricuspid valve repair with a four-grade rather than three-grade system, physicians can predict survival more accurately, reported investigators.
The severity of tricuspid regurgitation is usually classified as either mild, moderate, or severe. But when four grades are created by subdividing moderate tricuspid regurgitation into mild to moderate and moderate to severe tricuspid regurgitation, the survival curves separate meaningfully, according to Julien Dreyfus, MD, PhD, from the Centre de Cardiologie du Nord in Saint Denis, France.
A patient with mild to moderate tricuspid regurgitation is significantly more likely to be alive after 2 years than one with moderate to severe tricuspid regurgitation, said Dreyfus, who presented the findings here at the Congress of the European Association of Percutaneous Coronary Interventions 2024. The work was simultaneously published in JACC Cardiovascular Interventions.
A four-grade scheme is already recommended for evaluating regurgitation following mitral valve repairs.
Survival Differs in Moderate Risk Groups
Dreyfus and his team used data from TRIGISTRY, a tricuspid valve registry that has so far enrolled 2413 patients from 33 centers in 10 countries. The study looked at survival in the 613 patients who had an adequate assessment of tricuspid regurgitation following a transcatheter valve repair procedure and had complete follow-up. Each patient was assessed using first a three-grade and then a four-grade scheme.
Using the three-grade scheme, 203 patients (33%) had no mild tricuspid regurgitation, 319 (52%) had moderate residual tricuspid regurgitation, and 91 (15%) had severe tricuspid regurgitation at discharge. There was a statistically significant difference in survival between the moderate and severe groups but not between mild and moderate.
With the four-grade scheme, the moderate tricuspid regurgitation group, which represented slightly more than half the patients in the study, was divided into 201 patients (33%) with mild to moderate tricuspid regurgitation and 118 patients (19%) with moderate to severe tricuspid regurgitation.
In the four-grade scheme, there was no significant difference in 2-year survival between those with no or mild regurgitation and those with mild to moderate regurgitation or between those with moderate to severe and severe regurgitation. But there was a large and statistically significant difference between those with mild to moderate regurgitation and those with moderate to severe regurgitation: 80% vs 55%.
“These data show that the outcome of patients with moderate residual tricuspid regurgitation as conventionally defined are heterogeneous,” Dreyfus explained. “By subdividing the moderate tricuspid regurgitation into two different grades, it refines the prognosis of these patients.”
Ultimately, these results “support a more granular classification of tricuspid regurgitation in order to predict outcome,” he said.
Variations Also in Transcatheter Edge to Edge Repairs
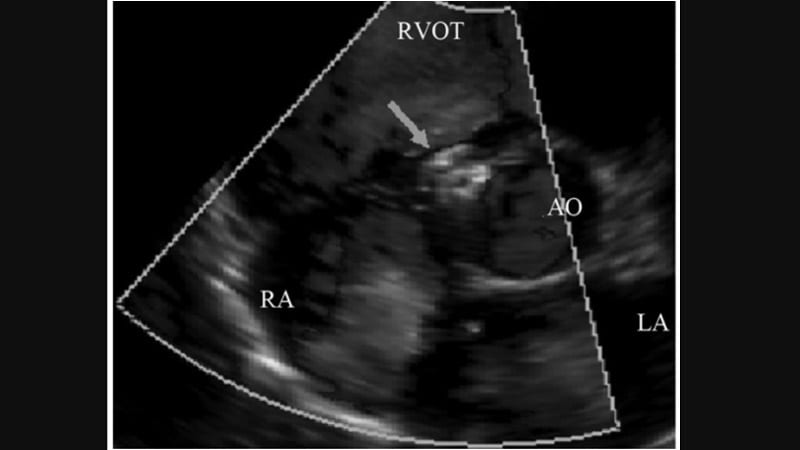
Among the patients undergoing a transcatheter repair in TRIGISTRY, most (79%) underwent a transcatheter edge to edge repair. Almost all the others (19%) underwent annuloplasty, although a few were repaired with different transcatheter techniques.
When the transcatheter edge to edge repairs were evaluated separately for 2-year survival, the separation was even greater between the mild to moderate and moderate to severe grades. Conversely, the survival curves for the no and mild tricuspid regurgitation and the mild to moderate tricuspid regurgitation were almost superimposable, with only a slight separation over the final 6 months of the analysis.
As a less invasive alternative to surgery, transcatheter tricuspid repair has become the dominant method of tricuspid regurgitation correction in several countries, Dreyfus said. He noted that other studies, including the recent TRILUMINATE trial, suggest that the transcatheter approach is safe and effective compared with surgery.
However, 30% or more patients still experience meaningful tricuspid regurgitation after transcatheter procedures, according to Dreyfus. So, a more granular assessment of tricuspid regurgitation would help better anticipate bad outcomes and provide an opportunity to consider additional interventions.
Paul Sorajja, MD, director of the Center for Valve and Structural Heart Disease at the Minneapolis Heart Institute in Minnesota and principal investigator of TRILUMINATE, said he was intrigued by this analysis but cautioned that it is difficult to distinguish between tricuspid regurgitation that is causing bad outcomes and tricuspid regurgitation that is merely associated with bad outcomes.
Sorajja pointed out that the survival curves in TRIGISTRY, unlike those in TRILUMINATE, began to separate within 1 year, raising the possibility that the protocols in the two sets of data differed and that controlled data are needed to further test a four-grade system.
Dreyfus acknowledged that several variables affecting outcomes were not evaluated in this study. He suggested more studies, particularly controlled trials, are needed to confirm the results, but given the prognostic value of four tricuspid regurgitation grades over three in this analysis, he said that “more granularity would be helpful” in evaluating residual tricuspid regurgitation for the potential of identifying patients at high risk for poor survival.










