Fitness
Food And Drug Administration Testing For Avian Flu In Dairy – Health Policy Watch

Amid the growing avian influenza epidemic in American cattle, the US Food and Drug Administration (FDA) launched new research Tuesday to ensure dairy products available in the market do not contain the virus in its active form.
The research will involve a series of studies to test pasteurised milk samples collected from store shelves. The study aims to determine if, and to what extent, virus contamination may occur in individual as well as pooled milk product samples, as well as in other diary products like cream and cheese.
The retail survey aims to cover geographic and product gaps in the sampling of 297 products in late April and early May, which found all products tested were H5N1-free.
“As outlined in the FDA’s research agenda released today, the FDA is working on multiple efforts to understand the effectiveness of pasteurization and other inactivation methods,” the FDA advisory stated. So far, pasteurisation proves effective but more research is needed to ensure the virus does not present risk to the food supply.
Farmers reluctant to agree to cattle surveillance
Since March, the highly pathogenic avian flu strain, H5N1, has infected 131 US dairy cow herds in 12 states, according to a separate update from the US Centers for Disease Control and Prevention (CDC). Three human cases of infection following exposure to infected dairy cows have also been reported.
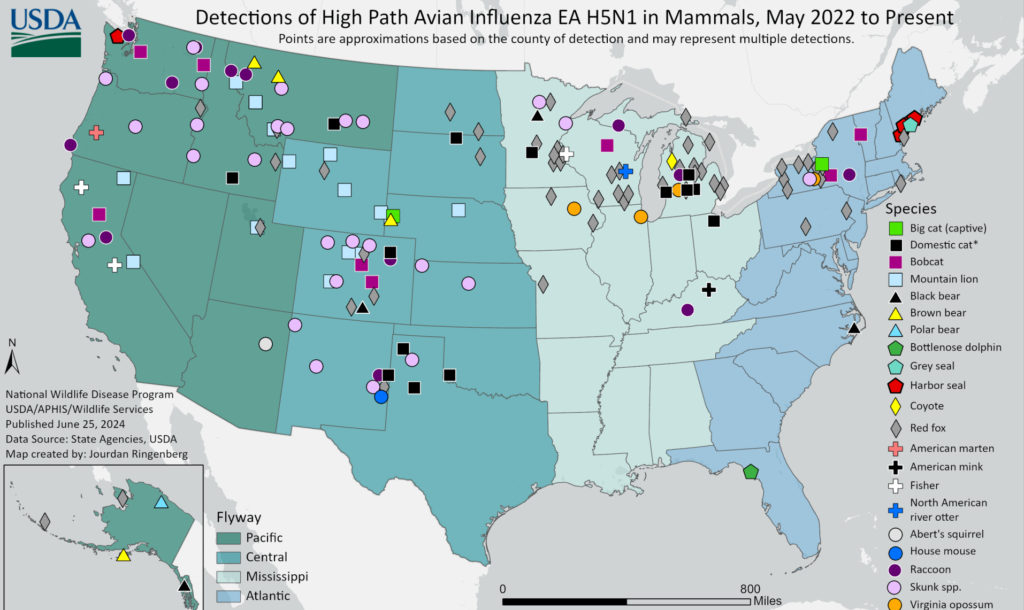
WHO has assessed avian flu risks to public health as low for the general population and low-to-moderate for people working with animals. Yet, as the virus gains ground infecting more species, the risk of human-to-human transmission rises. In the US case, for instance, some 21 cats also have been infected since March. CDC has warned that dogs could become another virus reservoir, increasing risks of transmission to humans, although this scenario remains unlikely for the moment.
“CDC monitors disease outbreaks, looking at […] surveillance in wild animals. […] Risk assessments are performed,” said Christine Oshansky of the Biomedical Advanced Research and Development Authority (BARDA) during a National Vaccine Advisory Committee meeting June 13.
Despite the CDC’s and other agencies’ efforts, the US epidemic response has been regarded by many experts as woefully insufficient to date.
Farmers are reluctant to have themselves or their herds tested – practices that remain voluntary. Farmers also have expressed resistance to using personal protective equipment during milking, when, most likely, infections occur.
Abiding with CDC and FDA guidelines has perceived downsides, while the positives are not as evident: goggles or respirators, recommended by the CDC, can be cumbersome in the humid and hot milking parlors and reporting just one infected cow marks the whole herd as potentially sick, meaning financial loss for the farm.
The net result has been that only 45 people, so far, have been tested for avian flu symptoms, despite the estimated million tests distributed across the country. Lack of testing means the real epidemic situation is largely unknown. “We’re flying blind,” assessed Dr. Jennifer Nuzzo, the Director of the Pandemic Center at the Brown University School of Public Health, told KFFHealth News last week.
Stockpiling for emergency
Dedicated vaccines, another element of the epidemic response, are also not yet ready. The FDA has so far approved three H5N1 vaccines: made by Sanofi, a GSK subsidiary, ID Biomedical Corporation of Quebec (IDB), and CSL Seqirus – all of which take several months to produce.
Other countries, for instance the United Kingdom, are also preparing stockpiles, while Finland is starting a vaccination programme designated for risk groups, using a vaccine against the H5N8 strain.

Seasonal flu vaccines, though only moderately effective in preventing avian influenza infections, can still be helpful, Dr Aspen Hammond, a technical officer at the WHO, said during an Epidemic Information Network seminar on June 6.
“It has been recommended to use seasonal vaccines, especially in […] healthcare workers, obviously, but also in people that are exposed to potentially infected birds, just to try to minimise them developing symptoms,” he said.
Vaccinating animals also has an important role to play, emphasized Ian Brown, Chairman of the joint World Organisation for Animal Health/Food and Agriculture Organisation network of expertise on animal influenzas, during the seminar:
“It’s a simple equation: you reduce the infections in domestic birds, you reduce the risk of spillover to wild birds, you reduce the risk of spillover to humans.”
Image Credits: Ashoka Jegroo, USDA, Oikeutta eläimille.
Combat the infodemic in health information and support health policy reporting from the global South. Our growing network of journalists in Africa, Asia, Geneva and New York connect the dots between regional realities and the big global debates, with evidence-based, open access news and analysis. To make a personal or organisational contribution click here on PayPal.










