Fitness
Idiopathic pulmonary fibrosis drug fails in phase 3 trial – UW Medicine | Newsroom
A promising drug for idiopathic pulmonary fibrosis (IPF) proved to be no better than a placebo at decreasing the rate of disease progression among participants in a multinational clinical trial. In earlier trials, the drug, pemrevlumab, had appeared to slow disease progression.
The results of the trial were published this month in JAMA, the Journal of the American Medical Association.
“Although the results are very disappointing, the completion of the trial in the midst of the COVID pandemic was a major accomplishment, said Dr. Ganesh Raghu, professor of medicine and director of the Center for Interstitial Lung Diseases at the University of Washington School of Medicine in Seattle. He was the paper’s lead author.
“The trials success was only possible because of the remarkable dedication of the patients and trial investigators who adhered to a difficult treatment protocol despite all the challenges posed by the pandemic,” Raghu said.
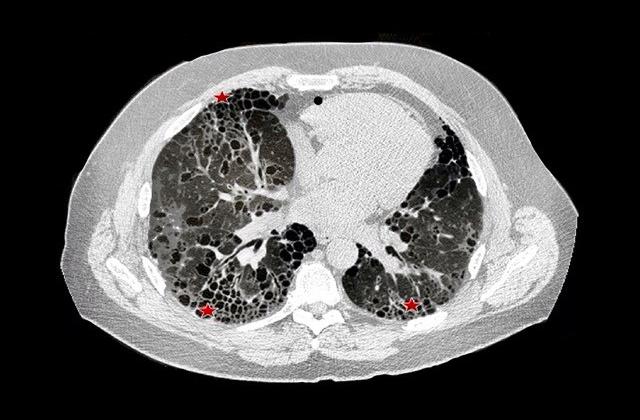
In IPF, normal lung is replaced by scar tissue, a condition called fibrosis. Lungs become stiff, as the disease progresses, and breathing becomes more difficult. Death typically stems from respiratory failure.
IPF’s cause is unknown. Genetics may play a role. Risk factors include a history of smoking, exposure to environmental pollution and having gastroesophageal reflux.
The disease typically develops after age 60 and is more common in men. Symptoms include gradual onset of cough, shortness of breath and fatigue. Without treatment the median survival is three to five years.
There is no known cure. Lung transplantation is an option for some patients.
Only two drugs, pirfenidone and nintedanib, have been approved by the U.S. Food and Drug Administration for IPF. Both slow patients’ decline in lung function, but not everyone who takes the drugs reports relief of symptoms.
The drug evaluated in the new study, pamrevlumab, is a monoclonal antibody that binds to and inhibits a molecule called connective tissue growth factor, which plays a key role in the development of fibrosis. In phase 2 trials, the drug slowed the decline in lung function and was well tolerated.
In the new trial, 356 patients were randomly assigned to receive either pamrevlumab or an inactive placebo intravenously every three weeks for 48 weeks. Changes in lung function were assessed with a test called forced vital capacity (FVC), which assesses the elasticity of lungs and their ability to expand. With IPF, elasticity declines as lung scarring progresses.
The researchers found that after 48 weeks of treatment there was no difference in the FVCs of patients who received pamrevlumab and those who received the placebo. There also were no significant differences in exacerbations of symptoms, hospitalizations or death.
Raghu said the failure of a drug that looked so promising underscores the recommendations of a recent report he coauthored.
To speed the identification and evaluation of new drugs, the report urged researchers to decrease the emphasis of lung function tests as primary outcomes and give more weight to improvements in patients’ symptoms and quality of life, he said.
“IPF trials should focus on patients’ experiences — how they feel, function and how long they survive — not just measures like FVC,” he said.
Written by Michael McCarthy










