Fitness
Phase 3 Study of Novel Immunotherapy Combo Offers Promise in Advanced Melanoma
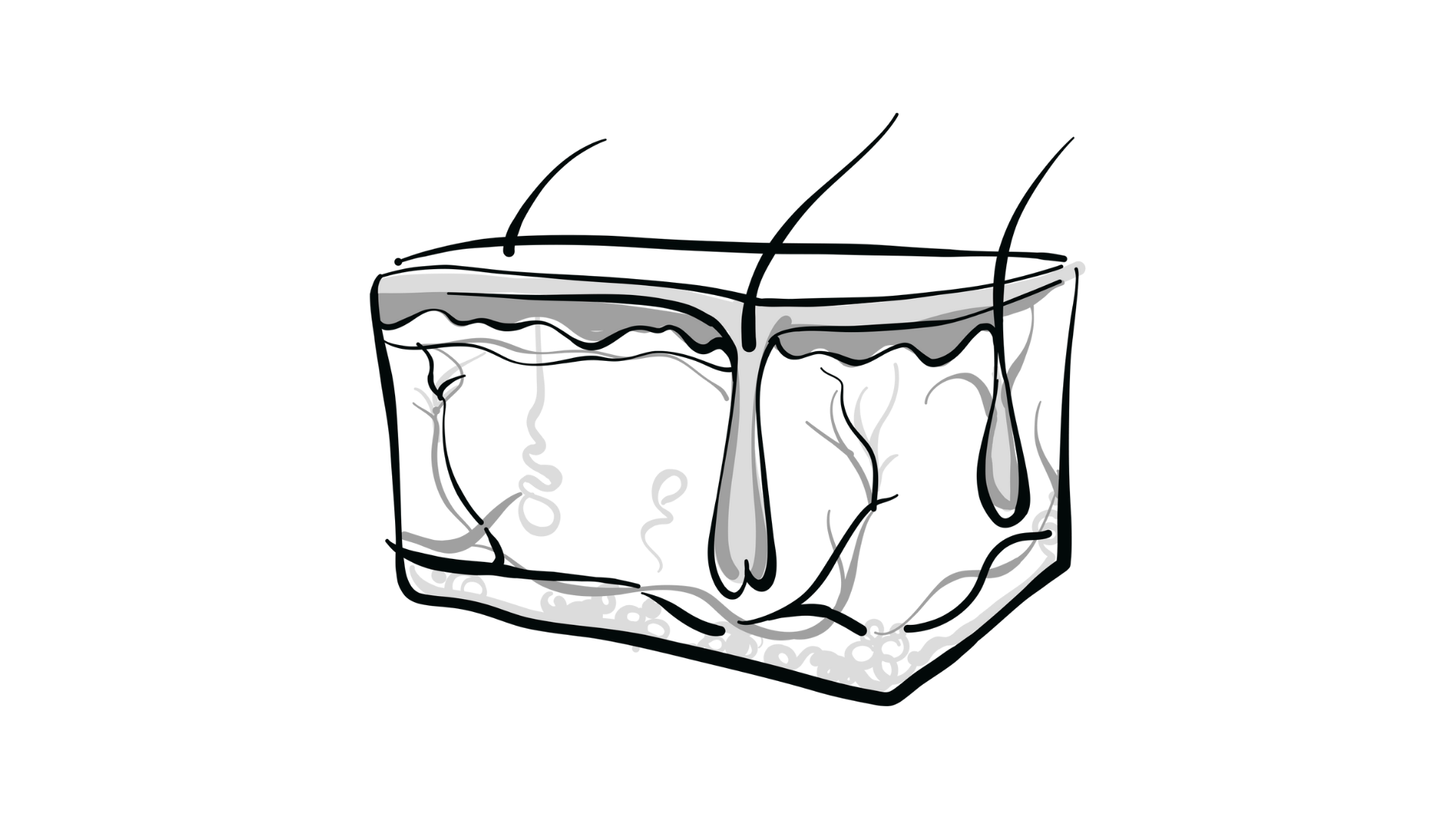
Cytological image of melanoma
While FDA-approved immunotherapy combinations exist for the treatment of advanced melanoma, several studies are committed to finding more effective treatments that deliver higher response rates. At the 2024 American Society for Clinical Oncology (ASCO) Annual Meeting, Nikhil Khushalani, MD, presented a poster for a phase 3 (NCT06246916) testing the effectiveness of a new drug combination in this intent-to-treat population.
The combination consists of fianlimab, an anti-LAG-3 agent, plus cemiplimab (Libtayo), an anti-PD-1 checkpoint inhibitor. Previous studies have suggested that blocking LAG-3 alongside PD-1 may be more effective than blocking PD-1 alone.
Phase 1 and 2 studies of this combination have showed promising results with manageable adverse effects.
This phase 3 trial is investigating this combination plus the established combination of relatlimab plus nivolumab (Opdivo). The primary end point is overall response rate, and secondary end points include progression-free survival and overall survival.
In an interview with Targeted OncologyTM, Khushalani, medical oncologist, senior member, and vice chair in the Department of Cutaneous Oncology at the Moffitt Cancer Center, discussed the study, its goals, and potential implications for patients with advanced melanoma.

Targeted Oncology: What are the unmet needs in this patient population this study focuses on?
Khushalani: Primarily, in the frontline setting for advanced melanoma, we have some very good treatment options. But these treatment options benefit approximately 50% of patients, which means there is an unmet need for patients who have what is referred to as primary refractory disease for advanced melanoma to checkpoint inhibitors. We are constantly trying to find ways to enhance the response rates, and more importantly, the durability and length of response, hopefully, trying to cure these patients or at least render them with durable disease benefit.
Could you explain how fianlimab works and how it could be useful in combination with cemiplimab?
This large, randomized, phase 3 trial is examining the experimental combination of fianlimab, which is an anti-LAG3 innovating antibody, in combination with cemiplimab, which is an anti-PD1 antibody. [Investigators are] comparing this combination to currently FDA approved combination of nivolumab plus relatlimab, which again, targets the same agent, so anti-PD1 [and] anti-LAG3. But the belief is that this combination may enhance response rates further. Currently, the response rate to the approved combination of [nivolumab] plus [relatlimab] is approximately 43%. That has been effective and more importantly, is tolerated well by patients. But with the newer combination, the hope is that we can further improve those response rates and possibly the durability of response.
What specifcially is the study evaluating?
This is a randomized, phase 3, open-label trial. A total of 560 patients are to be randomized between the 2 arms; 1 is the experimental arm and the [other is the] standard of care arm of [nivolumab] plus [relatlimab]. Patients have unresectable or advanced metastatic melanoma, therapy-naive for their metastatic disease. They may have received treatment for adjuvant therapy or neoadjuvant therapy; that will be 1 of the stratification factors. The other 2 stratification factors are the stage of disease, the extent in terms of metastases, and secondly, the presence or absence of an elevated serum lactate dehydrogenase [LDH], which is an important prognostic factor in this patient population. The standard of care arm gets standard dosing of [nivolumab] at 480 mg and relatlimab at 160 mg [in a] fixed-dose combination. The fianlimab and cemiplimab combination is also fixed dose [of] 1600 mg intravenously of fianlimab with 350 mg intravenously of cemiplimab every 3 weeks.
The primary end point is overall response rate that will be assessed after 400 patients have been randomized. The secondary end points are progression-free and overall survival, and that is after the full cohort of 560 patients have been randomized. Patients can continue treatment until disease progression and intolerable toxicity or patient and or provider preference or up to a maximum of 2 years of treatment.
What are some of the benefits and limitations of fixed-dose treatment regimens such as this?
I think the clear benefit of fixed dose is it is in 1 vial; it is 1 administration for patients. Certainly, it is convenient because there is no dose variability between patients. The obvious disadvantages that if a patient does indeed develop toxicity to treatment, it is hard to discern which of the 2 agents the toxicity is specific to and which 1 potentially can be dropped. For example, in 1 of our existing combinations that we use very frequently, which is ipilimumab [Yervoy] plus nivolumab, if a patient does have grade 3 or higher toxicity, often we will drop the ipilimumab for future treatment and continue with nivolumab. The anti-PD-1 agent here becomes a little bit harder to discern that, but we will have to then drop the fixed-dose combination and continue with nivolumab alone as a potential option.
Do you have any sense of the tolerability of this new combination?
Cemiplimab by itself is tolerated well. We know that based on this approval in other disease states, including, for example, cutaneous squamous cell carcinoma that is unresectable, the combination of cemiplimab plus fianlimab was also well-tolerated, and no unusual safety signals have been observed in the earlier phase 1/2 trials, where we noted a high response rate with that combination of 61% to 62%, and [it was] well-tolerated from that standpoint. We do not anticipate any unusual safety signals,but we would like to test this in a larger patient population.
Have there been any previously observed efficacy findings?
I think what is unique about the combination is that in the preceding trials that led to this phase 3 study, responses were even seen in patients who had previously been exposed to anti-PD-1 therapy in the adjuvant or neoadjuvant setting, which is important because that is real-world. This is what we treat our patients now with; many of them will have already received single-agent anti-PD-1 therapy in the adjuvant setting, and then hopefully getting a combination that has now demonstrated efficacy. The other group that has demonstrated efficacy is in patients who have metastases to the liver, [which is] traditionally a harder-to-treat population as well as patients who have an elevated LDH level, again, an adverse prognostic factor.
Do you have any takeaways for colleagues?
I think the important takeaway would be this is real-world experience testing a new anti-PD-1/anti-LAG3 combination, going directly against an existing anti-LAG3/anti-PD-1 combination. We will certainly encourage our colleagues and other providers to refer patients. This is going to be a real-world community-based accrual, so up to 80 sites in the United States. We anticipate that accrual will be robust, and hopefully it can be contributed to by our colleagues.










