This transcript has been edited for clarity. For more episodes, download the Medscape app or subscribe to the podcast on Apple Podcasts, Spotify, or your preferred podcast provider.
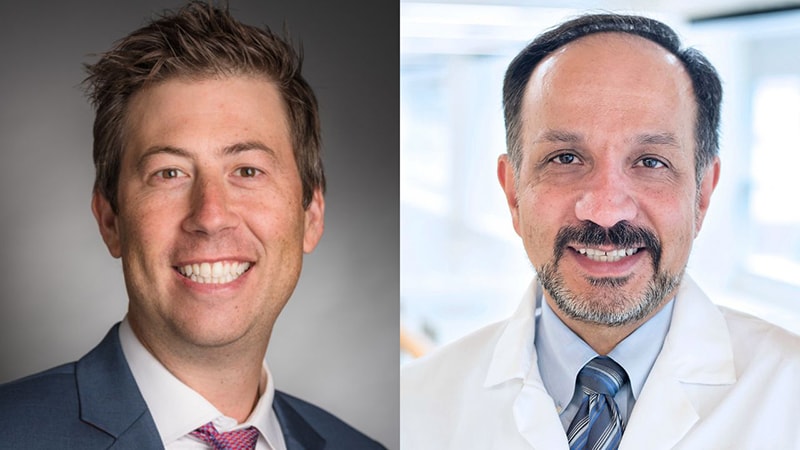
Jacob Sands, MD: Hello. I’m Dr Jacob Sands. Welcome to season three of the Medscape InDiscussion: Lung Cancer podcast series. Today we’ll discuss small cell lung cancer and some of the important advances in the field. First, let me introduce my guest, Dr Hossein Borghaei. Dr Borghaei is chief of the Division of Thoracic Medical Oncology, professor in the Department of Hematology Oncology, and Gloria and Edmund M. Dunn Chair in Thoracic Oncology at Fox Chase Cancer Center. Welcome to the Medscape InDiscussion podcast.
Hossein Borghaei, DO, MS: Thank you so much. Great to be here with you.
Sands: Dr Borghaei, I’d like to start out with something that is not necessarily brand-new data, but it is a change in the field that was pretty dramatic in the incorporation of immunotherapy in the first-line setting with platinum/etoposide. We saw IMpower133 and CASPIAN with atezolizumab and durvalumab, respectively, that became part of first-line therapy. Those were published in 2018-2019. We saw no substantial difference in median progression-free survival (PFS) and a 2-month benefit in median overall survival (OS). Why is this so game-changing and so important in the first-line setting?
Borghaei: Simply because it’s been nearly 30 years that we’ve made any kind of improvement in OS in metastatic small cell lung cancer. I often say that if you go back to the study of carboplatin/paclitaxel with or without bevacizumab in non–small cell lung cancer, the ECOG study that changed OS by 2 months, back then it was a big change because we hadn’t been able to improve on platinum doublet in non–small cell lung cancer. Now we have a very similar scenario with a disease that is very aggressive, and we’ve been using the same platinum doublet chemotherapy for two to three decades; all of a sudden, with the introduction of checkpoint inhibitors, we have an improvement of about 2 months or so in OS. We were all happy that we were able to make some dent. But I think what you’re hinting at is that it is not as significant of an improvement as we would want to see. However, for this disease, even some incremental improvements are welcome news. I think that the excitement had to do with the fact that, again, in an intent-to-treat patient population, we were able to improve OS, and we hope that we can build on that. I think that was the excitement and that’s why everybody keeps talking about those two studies. The standard of care has basically changed with the two presentations.
Sands: The surprising thing within it is the tail of the curve where we see these durable responses. I think many of us now, or those who are treating enough patients with small cell lung cancer, are seeing some of these patients who are years out from their initial diagnosis. I have a handful who are now more than 5 years from their initial diagnosis, which was really unheard of before. But it’s not enough. In both of these trials, the treatment was ongoing. Is there a point at which you’re then stopping these immunotherapies or do you do that for years, indefinitely?
Borghaei: I haven’t been as fortunate as you are in having a number of patients going as far out (with durable responses). My experience is that the majority of the patients who are on checkpoint inhibitors end up experiencing significant fatigue and some other side effects, and, because of the quality-of-life issues, we have had to hold treatment or discontinue treatment on a number of our patients and just follow them. I agree with you that the tail of the curve is really interesting. But the unfortunate thing is that we still haven’t been able to identify upfront who those patients are who might maximize benefit from a checkpoint inhibitor. Of course, as you are really very well aware, there are data that, perhaps, the inflamed subtype of small cell lung cancer could be a group of patients who could be benefiting from treatment with a checkpoint inhibitor. Whether that is a fact that we can establish in a randomized, prospectively designed study or not remains to be seen. I agree that there are definitely patients who have benefited from a checkpoint inhibitor. I have a patient who I think is a long-term responder with really good disease control on the original ipilimumab and nivolumab study. There are those patients out there. I think the challenge is, how do you identify that patient population upfront? What is it about those specific tumors or patient characteristics that we can learn from, and is that something that we can build on to elevate the tail of the curve, to include more patients who could benefit from these combinations? To my knowledge, we haven’t really been able to truly establish that particular subgroup and have that coveted biomarker identified for that patient population.
Sands: It’s such an important point. You have a drug that could be a home-run drug for somebody, but there’s a higher likelihood that it’s not going to be effective for an individual. It’s a subset that has overwhelming benefit, it seems. I’ll say that’s part of why I think it’s so important to give it in the first-line setting, where they have a shot at that while they’re also getting platinum/etoposide, where the majority of patients have a response to that, so they’re going to be captured. That raises the next topic. Initially, pembrolizumab and nivolumab were FDA approved and had accelerated approval in the third-line setting. This was as single-drug therapy. The slope of that curve was a pretty steep drop-off. But in the pembrolizumab studies, for example, there was a 19% response rate, but 13% with ongoing response at 2 years. A remarkable outcome for that 13% of patients. But 81% didn’t respond to therapy. Due to this, I think of pembrolizumab or nivolumab as being an important drug to consider in those who never got a checkpoint inhibitor. For the most part, that’s someone who had limited-stage disease, got treated with chemotherapy and radiation, and now has recurrence. Are you considering pembrolizumab or nivolumab in that setting? I imagine that if it has been more than 6 months, doing platinum/etoposide plus atezolizumab or durvalumab is the easier answer. But let’s say, for whatever reason, that you’re not doing that; are you considering single-agent pembrolizumab or nivolumab?
Borghaei: I’ve definitely considered that. I’ve discussed it with patients. I think it’s interesting how the approvals were actually withdrawn — or the use of the drug was actually withdrawn — because I agree with you on the 19%-20% response, some of them being durable. Again, with all the caveats that we’ve discussed, we don’t know who the patients are and how to select them. I was surprised that we were not able to have access to these drugs in the second-line setting. What do you do with the patient population that you are describing, with chemoradiation and short-interval disease progression? I think checkpoint inhibitors can have a role in that setting. The question now, of course, is, how do you get access to it? I do consider it for exactly the patient that you are describing here. I do try to at least get patients introduced to the checkpoint inhibitors. I agree with you that if it is prolonged PFS and you have the opportunity to repeat the platinum/etoposide, it’s just an easy transition to do chemotherapy plus immunotherapy. But I agree with you. I do consider single-agent immunotherapy in the patients who cannot be re-treated with a platinum/etoposide.
Sands: In the second-line setting, small cell lung cancer becomes a different diagnosis. I’d say that in the first-line setting, a majority of patients respond to platinum-based therapy. There are some really long-term responders, as we’ve said, with the incorporation of immunotherapy. The second-line setting is where resistance becomes much more real, and the durability tends to really shorten, from what we’ve seen. For a brief overview, topotecan has been a longstanding second-line approved therapy. This was initially approved as an infusion after a publication in the JCO in 1999 — that was vs cyclophosphamide, doxorubicin, and vincristine (CAV). The curves overlap each other entirely, but there was better symptom improvement in the topotecan arm, therefore leading to FDA approval. Of course, we also saw another publication in 2006 that was the oral (PO) form of topotecan vs best supportive care, showing a partial response rate of 7% and 44% of patients having stable disease, and a median OS of about 6 months. There was better symptom control on the topotecan arm vs best supportive care. That led to the PO FDA approval. More recently, in 2020, we had the basket trial of lurbinectedin that showed a response rate of 35%, and another 33% with stable disease and a median PFS of 3.5 months. In the group with a less than 90-day chemotherapy-free interval, the platinum-resistant group, we saw a 19% 6-month PFS. So that is a better response in the second line, or a more durable response in the second line, than in the first line for about 1 in 5 patients in that group, and 43% 6-month PFS in the more platinum-sensitive group. The toxicity profile was pretty good for lurbinectedin, I thought. There was a 46% grade 3/4 neutropenia, but patients were not allowed to have primary prophylaxis. There was a 7% grade 3 fatigue, which in my experience seems about accurate. Based on that data, what do you tend to use as your second-line therapy? What is your second, third line? I can mention irinotecan because some people use irinotecan rather than topotecan. How do you go about treating patients in second and third line? What is your thought process on that? What is your strategy?
Borghaei: I think it’s a bit of an evolving area and an area where we are desperately in need of additional drug development and treatment. I’ll be up-front and say that for some of the stuff that we’re about to discuss, I’ve been either an investigator or continue to be an investigator in these drugs. In full transparency, I’ve consulted with a number of companies. To be honest with you, I have been using lurbinectedin quite a lot in the second- and third-line settings. If I have a patient who can be described as platinum sensitive, I’ve been using the platinum-sensitive patient population, who go back to the platinum/etoposide, and try to use that again. That’s a difficult treatment for patients to tolerate. Myelosuppression, neuropathy, allergic reactions to carboplatin — all of these things are there, but it is a good, valid treatment option for patients. Short of that, I’ve tried to avoid topotecan and use more lurbinectedin at the time of progression, simply because I think, at least in my experience, patients tolerate it a little better than topotecan. The myelosuppression is real. I don’t think it is quite as severe as what I used to see with topotecan. We use a different schedule of delivery with topotecan. The standard 5-day was always there and always toxic. I think there are publications from the ovarian cancer group using it on a weekly basis. We used some of that in some patients in the old days. I didn’t really like the PO topotecan approach quite as much, but I do understand that some of our colleagues have used it quite extensively. That was the experience with topotecan, and again, as you just suggested, the approval was mostly based on quality-of-life improvement, not so much a lot of the clinical efficacy endpoints that we’re used to seeing nowadays. Even though I don’t think lurbinectedin has the required randomized phase 3 study, you have to have comparisons. In general, I would say that in my clinic, the clinical efficacy and toxicity have been pretty consistent with what has been reported so far with the drug. I’ve preferentially been using this agent in that setting.
Sands: I think what you’re describing is something I consistently hear across the country. The other thing about lurbinectedin is it’s once every 3 weeks. Sometimes I’ll talk about time toxicity where, for topotecan, if it is once a day for 5 days in a row, that’s quite a bit more time. I know you said that sometimes there are people who will dose it differently, but that’s the approved dosing. You said you use lurbinectedin as second line. Is topotecan something you use in the third line or do you use irinotecan? I tend to use irinotecan rather than topotecan, but I know there’s broad variation in that and there are some people who are very confident and comfortable using topotecan as well.
Borghaei: I’ve definitely gone to topotecan in the third-line setting in the absence of clinical trials and other options that we sometimes have for patients. Even though we don’t have a lot of data for it, I have to admit that in the third-line setting, sometimes I have used agents like paclitaxel, which has some clinical activity associated with it in the world of small cell lung cancer. If I am faced with a patient who might suffer from significant toxicities, especially myelosuppression with topotecan, and that it could cause additional issues, then I have, again, preferentially used paclitaxel even on a weekly basis for the management of patients in the third- or fourth-line setting.
Sands: We’ll come back to paclitaxel, but let’s maybe sidetrack for a moment on the myelosuppression that you mentioned with topotecan. We see myelosuppression with platinum/etoposide. We now have trilaciclib approved for myelosuppression in those receiving a platinum/etoposide or topotecan regimen. In small cell lung cancer, the data did not result in any real changes as far as efficacy in treating the cancer, but it did show substantial, significant reductions in cytopenias — the primary endpoint of these studies being neutropenia. Although, frankly, to me, the value is not just that, but more so the anemia and thrombocytopenia, because it works across all cell lines, as opposed to the drugs we’ve had around, which have really been neutropenia focused. One of the things that I thought was most compelling is something that Jared Weiss has talked about, in that the improvement in quality-of-life outcomes, particularly around fatigue, also seems to correlate with improvements in anemia and makes me realize that there probably is some degree of fatigue that is attributable to anemia that I’ve likely underappreciated, because these drugs cause fatigue as well. They cause anemia. We say, okay, there’s some anemia, but not enough that we would give a transfusion. But maybe if there was less of that, patients would actually have less fatigue and therefore feel better as well. I still don’t use this for everybody, but it has been something that I’d certainly consider in everybody, depending on the circumstances. Can you walk us through some of the nuance of your thoughts around trilaciclib? What did you think of the data, and has it affected your practice?
Borghaei: That is a great question, and I think our practices are very much in tune. I’m not using it in everybody. I have to say that I am a recent converter, and the primary reason was a patient in clinic where we were faced with significant anemia and myelosuppression, despite the use of growth-factor support in this particular patient. I have to say that I wasn’t really all that impressed with the data initially. I’ve looked at it. I thought that this might be an additional expense that we’re adding to a regimen that works really well. We’ve been managing neutropenia with the standard growth-factor support that we’ve had. This particular patient taught me a valuable lesson about the use of this particular drug. I’ve really been happy that I’ve been able to use that because we’re faced with a shortage of blood products throughout the country. We’ve lowered the hemoglobin level for patients who qualify for receiving blood transfusion simply because of all the need that’s out there, and I wouldn’t discount the impact of anemia and the fatigue that goes with it — in particular for a patient population that usually has additional issues, cardiovascular respiratory issues, because the majority of these patients could have emphysema, chronic obstructive pulmonary disease, and other issues. I think it actually is something that we should take a little more seriously, because from a quality-of-life point of view, the fatigue that’s associated with anemia is significant. I am a recent converter. We’ve had the drug in our formulary. I have a couple of patients who are receiving this agent along with their chemotherapy. It’s a bit of a disappointment that we don’t necessarily see an improvement in clinical efficacy the way we want to. One would’ve thought that being able to stay on schedule and on time with the delivery of chemotherapy, with the prescribed doses, would’ve had an impact on clinical efficacy. Hopefully there will be additional information down the road that would help us in that regard. For specific patients, just as you said, not for everybody, I am happy that we have access to this particular drug. I think additional information or studies are needed to really establish its place in the everyday clinical practice. Like with many other drugs that we get nowadays, it’s hard to give a blanket statement saying anybody who walks in through the door should be a candidate for X or Y. I think we have to be careful how we pick and choose who is offered the particular treatments. I’m happy so far with the drug and I am using it in select cases.
Sands: I am similar, although I’ve also looked back and thought that it showed improvement in health-related quality of life. That’s obviously important. We highlighted that topotecan got FDA approved on improvement in patient symptoms, and now other drugs we say failed against topotecan when they didn’t show superiority — although, frankly, topotecan didn’t show superiority in getting FDA approval either, except for maybe the PO form, which was vs best supportive care and against no cancer-directed therapy. I don’t think it’s something for everybody, but my threshold for using it has certainly been lowered. I do think those patient outcomes are a very important consideration. You brought up paclitaxel earlier. As we get into the third, fourth line of therapy, the tolerability of these regimens becomes particularly important. I agree with your comment earlier that weekly paclitaxel is very well tolerated. I dose that 6 weeks on, 2 weeks off. There’s temozolomide, which is a pill form, and that’s something that I consider particularly in patients with central nervous system disease. My answer is similar to what you had mentioned earlier.
Clinical trials, or when patients qualify for trials — there is so much going on in the small cell lung cancer space that I want to make sure we really have some time to discuss this. We saw that highlighted in The New England Journal of Medicine with tarlatamab, a DLL3 bispecific T-cell engager, so it binds CD3 on T cells. The 10-mg dosing showed over 40% response rate with quite a bit of durability and was generally pretty well tolerated. There was some early cytokine release syndrome, pretty much grade 1/2, and some neurotoxicity as you get into cycle 2. Can you take us through the data a bit more and give us your thoughts about tarlatamab? And then we’ll use that as a launch into DLL3-directed therapies in general.
Borghaei: I’d be happy to. I am an investigator on the tarlatamab study, from phase 1 onward, so I do think that the drug is an interesting addition — once approved, of course; it is still under investigation. It should be considered investigational when used in the clinical trial setting. This is a drug that I’ve had a lot of interest in just because of its bispecific nature. By definition, these are bispecific T-cell engagers, as the name suggests and as you said, so one arm of the drug directly engages the CD3, and the other arm of the study obviously goes after a tumor antigen — in this case, DLL3. Many of the listeners are familiar with the fact that DLL3 has been around for a while. We’ve had other drugs targeting DLL3 in the past, some with success and some without. The target is a relevant target in the world of small cell lung cancer, based on a lot of the preclinical work in some clinical trials. You can think of bispecific T-cell engagers as bringing the immune system and the tumor in close proximity and generating what we used to call in the old days an immunologic synapse, so to speak. The idea here was that with the two arms, you can sort of bring the whole immune component into the tumor microenvironment, hoping for a better immune response. The New England Journal of Medicine article examined two different doses of this drug. Both doses come from the phase 1, like in any other study. But on the phase 1 clinical trial, a multitude of doses were investigated in multiple cohorts, going all the way to a 100-mg dose. The question here was, what was the clinical efficacy of the higher dose vs the lower dose? Having treated a number of patients at our institutions on this trial, I have to say that I’ve been very happy with the responses. And again, as you correctly pointed out, the durability, because we get a lot of drugs in the world of small cell lung cancer where you might have an initial response but unfortunately the durability isn’t there. At least so far, there were 220 patients in that New England Journal article with the two doses of the drug. We’re beginning to have a relatively healthy dataset of patients in terms of clinical data and toxicity. The response rate of 40% with a 10-mg dose is very interesting, considering that these patients were pretreated. In the phase 1 trial, the response rates were a little bit lower. About 30% of patients on the phase 1 had multiple lines of prior therapy, some of them beyond three lines of treatment, which is a unique situation in small cell lung cancer. I don’t know how you think about this, but yes, they’re heavily pretreated, but it’s also a rare patient population with small cell lung cancer that can go three lines of treatment and beyond and still have a good-enough performance status and other factors that we require for participation in a clinical trial. In the world of small cell lung cancer, I think we have to be careful what we’re talking about when we say “a lot of third-line–and–beyond patients.” It still matters, but nonetheless, the drug does show decent durability as a single agent, and interesting enough, the OS as reported — obviously, additional work is needed.
Sands: We’ve highlighted the efficacy, which of course is very important when talking about a new drug. Now let’s transition a bit to the toxicity profile. We saw some cytokine release syndrome. We also saw some neurotoxicity. Can you talk a bit about that profile and what you think of side effects looking forward with this drug?
Borghaei: The toxicity, because it’s a T-cell engager, is real. The cytokine release syndrome can occur. As you pointed out, a majority of these were grades 1 and 2. From a physician point of view, a resource point of view, we’re sort of trained to look at grades 1 and 2 as being manageable by physician criteria. Obviously, from a patient point of view, that’s a different matter. Nonetheless, I think it’s important to realize that many of these were managed without a need for prolonged hospitalizations or anything like that. The neuro issues that you brought up are also important, and we do have to pay attention to all of these adverse events and figure out how to mitigate some of these. Overall, I’m kind of interested in this class of drugs, and there are two or three other bispecific engagers that are now going through the clinical trial evaluation process. We’ll eventually see what these drugs’ place will be, whether it’s strictly in the second line, whether it can be moving to the front line and what the ramification of all of that is. Hopefully we’ll have access to more drugs with good response and durability for a patient population that is in desperate need of additional treatments. Overall, I’ve been very encouraged with what we’ve seen.
Sands: I thought it was exciting data, to see a pretty high response rate and the durability and general tolerability. We also have the Harpoon trispecific T-cell engager and the Boehringer Ingelheim T-cell engager. There’s a class of drugs that seems to be showing some efficacy. Then there are other drugs in development that are DLL3 directed on top of some antibody-drug conjugates. There’s really so much more to discuss, so when we get back together in the next year or two, I think there will be a lot more to update on. Unfortunately, that’s all the time we have to discuss small cell lung cancer advances. Today we’ve talked to Dr Hossein Borghaei. Thank you for tuning in. Please take a moment to download the Medscape app to listen and subscribe to this podcast series on lung cancer. This is Dr Jacob Sands for the Medscape InDiscussion: Lung Cancer podcast.
Listen to additional seasons of this podcast.
Resources
First-Line Atezolizumab Plus Chemotherapy in Extensive-Stage Small-Cell Lung Cancer
Paclitaxel-Carboplatin Alone or With Bevacizumab for Non-Small-Cell Lung Cancer
Pembrolizumab for the Treatment of Non-Small-Cell Lung Cancer
Tarlatamab for Patients With Previously Treated Small-Cell Lung Cancer