Fitness
The role of genetic testing in cancer immunotherapy | News
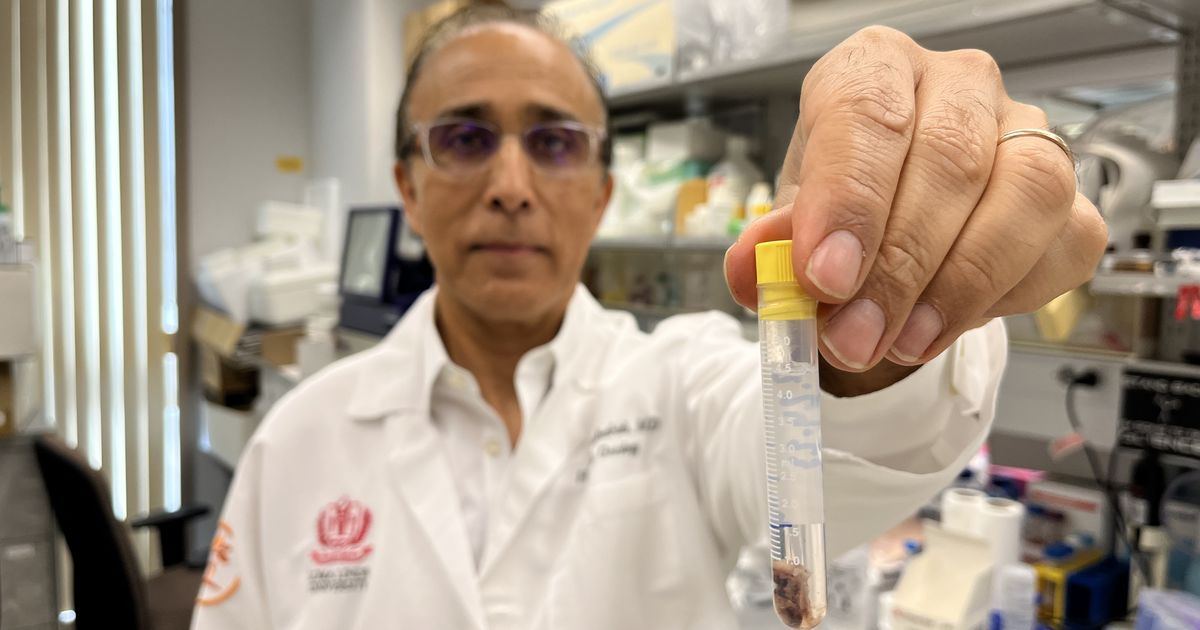
Loma Linda University Health’s Cancer Center is at the forefront of advancing cancer treatment, focusing on the burgeoning field of immunotherapy. Hamid Mirshahidi, MD, division chief of hematology-oncology, offers insights into the critical role of genetic testing in enhancing the efficacy of cancer immunotherapy.
Genetic testing has emerged as a cornerstone in personalized cancer treatment, offering profound implications for immunotherapy, he says. Two primary types of genetic tests are used in cancer care: germline and somatic (or tumor) genetic tests.
- Germline Genetic Testing: This test examines an individual’s inherited genes to identify mutations that may predispose them to certain types of cancer. Germline genetic testing involves analyzing the individual’s DNA to see if they have any inherited mutations that could increase their risk of developing cancer. Mirshahidi says knowing a patient’s genetic predisposition helps in the early detection and prevention of cancers, making it a pivotal tool in precision medicine.
- Somatic (Tumor) Genetic Testing: This type of testing is conducted on the cancer cells to identify genetic mutations driving the cancer’s growth. “Tumor genetic testing tells us what specific genetic abnormalities are present in the cancer cells, which can guide us in choosing the most effective targeted therapies,” Mirshahidi says.
The integration of genetic testing and immunotherapy
Immunotherapy leverages the body’s immune system to fight cancer, and genetic testing is vital in optimizing these treatments. The immune system has two main components: the innate immune system and the adaptive immune system. The innate system provides a general defense against pathogens, while the adaptive system targets specific threats based on previous encounters. Cancer cells often develop mechanisms to evade these immune defenses.
“Genetic testing helps us understand these mechanisms,” Mirshahidi says. “For instance, certain tumors express proteins that allow them to hide from T-cells, the immune system’s soldiers. By identifying these proteins through genetic testing, we can employ targeted therapies to block these evasive tactics, thereby making the cancer cells vulnerable to immune attack.”
Types of immunotherapies guided by genetic testing
- Checkpoint Inhibitors: These drugs release the brakes on the immune system, allowing T-cells to attack cancer cells more effectively. “One of the well-known biomarkers we look for is PD-L1,” Mirshahidi says. “If a tumor expresses PD-L1, it can be targeted with checkpoint inhibitors, which have shown significant efficacy in treating various cancers. The higher PD-L1 expression may translate to better response to check point inhibitors.”
- CAR T-Cell Therapy: This innovative treatment involves modifying a patient’s T-cells to recognize better and destroy cancer cells. Genetic testing helps identify the specific targets of cancer cells that CAR T-cells can be engineered to attack.
- Bi-specific T-Cell Engagers (BiTEs): These direct T-cells to cancer cells, bridging the immune and tumor cells. Mirshahidi said BiTEs require precise identification of tumor markers through genetic testing to ensure they bind correctly to the cancer cells.
“When patients understand how their genetic information guides the choice of therapy, they are more likely to participate actively in their treatment plans,” he says. “We explain to patients the different types of therapies and how genetic testing informs these approaches, making modifying the immune system less daunting.”
Future directions in cancer treatment
The integration of genetic testing with immunotherapy is poised to revolutionize cancer care, paving the way for highly personalized treatment strategies. As advancements in genomic research continue, the ability to pinpoint specific genetic mutations driving cancer growth will enhance the precision and efficacy of therapies, Mirshahidi says. He says future cancer treatments will likely see a shift toward these targeted approaches, reducing reliance on traditional methods such as chemotherapy and radiation, which often come with significant side effects.
The collaboration between genetic insights and immunotherapy holds promise for improving patient outcomes and creating tailored treatment plans that maximize effectiveness while minimizing adverse effects, ultimately transforming the landscape of oncology.
Learn more about treatments, programs, and research at Loma Linda University Cancer Center. Contact us at TCT@llu.edu or 909-558-9602 for new referrals or inquiries.










